MM Office Co., Ltd. Representative Director
Takashi Kudo
Graduated from Nihon University's School of Economics in 1982. After working in hospitals for 18 years, including as Chief of Medical Affairs at Kahoku General Hospital, Chief of Medical Affairs at Kameda Morinosato Hospital, and Head of the Corporate Planning Office, he has been in his current position since 1999. He specializes in planning hospital management strategies from the perspective of medical fees. He has clients in over 20 hospitals nationwide, ranging from 700-bed regional medical support hospitals to care mix hospitals with fewer than 100 beds. He has also Serialization numerous serials, including an opening column in Nikkei Healthcare (Nikkei BP).
The new medical fee revision for fiscal year 2024 will come into effect on June 1. In addition to various revisions to the new fee items, the new "community comprehensive medical ward admission fee" has been established, showing a new path for ward reorganization, which hospital management consultant Takashi Kudo calls super major. We asked him about these points and his advice to acute care hospitals that are being forced to reorganize their wards.
As you know, 2024 will be a year of triple revisions to medical fees, nursing care fees, and the Welfare Act for Persons with Disabilities. In addition, various reforms will be implemented with an eye on "Post-2025 (an increase in the elderly and a high death rate society until 2040)," including the implementation of work style reforms for doctors, clarification and coordination of outpatient functions based on the outpatient medical plan of the 8th Medical Plan, and the implementation of the 9th Nursing Care Insurance Business Plan. The 2024 medical fee revision will be linked not only to nursing care fees and the Welfare Act for Persons with Disabilities, but also to these reforms, and if it were expressed in a single kanji character, "tsunagu" (connect), which means to connect, would be the most appropriate.
With this as a background, the current revision of medical treatment fees has one pillar that runs through the entire range of stages, from the highly acute stage to the recovery stage, chronic stage, and home medical care and nursing care. At every stage, "cooperation between medical care and nursing care" is a given, and furthermore, support for "oral care, nutrition, rehabilitation, and dementia care" is required at every stage.
Meanwhile, acute care hospitals will be most affected by the review of basic inpatient fee requirements. After the last revision of medical fee remuneration in 2022, the number of hospital beds calculated as acute general inpatient fee 1 (7:1 nursing staff ratio) increased by 3,300 nationwide. The main reasons for this include: 1) the incorporation of community comprehensive care wards (hereinafter referred to as local care) was prohibited under the acute care enhancement system surcharge, so local care was returned to inpatient fee 1, and 2) to avoid the deduction introduced to the local care inpatient fee, local care was returned to inpatient fee 1.
This review of the basic hospitalization fee positions hospital beds that are charged the acute general hospitalization fee 1 as being the acute care beds, and the revision essentially eliminates wards that do not meet the new standards. A simulation by the Ministry of Health, Labor and Welfare showed four proposals that are expected to reduce the fee by about 10 to 20 percent. At the same time, the creation of a new hospitalization fee emerged at the end of last year, and a new "community comprehensive medical ward hospitalization fee" was established. The report's accompanying opinion clearly states that in light of this new establishment, "reorganization will be considered" after clarifying the function of the acute general ward with a nursing staffing ratio of "10 to 1."
In other words, this medical fee revision has set a new course for ward reorganization, and it is a major revision that creates new hospitalization fees. Beds with hospitalization fees of 2 to 6, other than acute general hospitalization fee 1, will likely be reassigned to "community comprehensive medical wards" and "community comprehensive care wards" over the next few medical fee revisions.
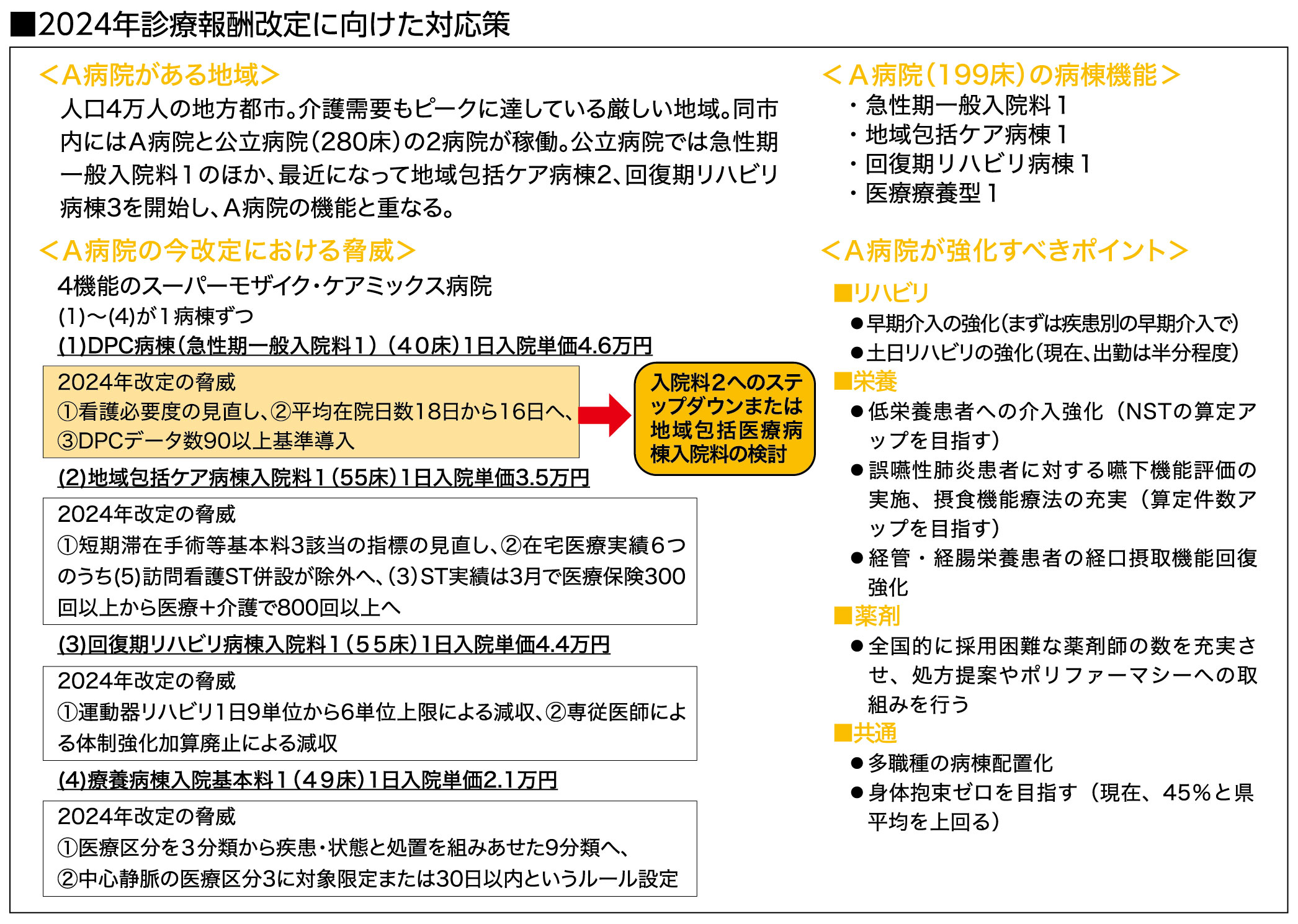
In light of the 2024 medical fee revisions, what each acute care hospital needs to do is review their ward organization and decide which hospitalization fee to choose by the end of September, when transitional measures such as nursing care necessity end. In particular, so-called "acute care hospitals" with low hospitalization costs are unlikely to be able to meet the new nursing necessity standards for acute general hospitalization fee 1, so a business decision is required. As a model, we will show the example of a care mix hospital A (199 beds) with four functions, so please use it as a reference.
When considering ward reorganization, it is important to clarify the role and function of your hospital, taking into consideration the local medical care system and the competitive situation. Depending on the choice you make, you may have to change your vision (how things should be). However, there is a tight time frame to come up with a new vision by the end of September, given the trends of other hospitals, so it is wise to get by with a method that is easy to change for the time being, and then consider ward organization based on the new vision in the medium to long term.
On the other hand, every time medical fees are revised, we hear complaints from the medical field that "even if we work on notified medical care (surcharges) and team medical care, it is not profitable." However, surcharges are messages (policy guidance) from the Ministry of Health, Labor and Welfare, and they provide incentives (rewards) for what medical institutions should do. Medical institutions that do not do what they should do (do not report surcharges) will likely have more losses. It is also important to understand that the purpose of team medical care is to improve the "quality of medical care" and task shifting is to improve "labor productivity."
In any case, in order to overcome this major revision of medical fees, it is important to respond appropriately by looking at the overall medical fees from the perspective of medical policy, demographic trends, and trends at other hospitals, rather than simply looking at the number of points.