In 2019, Omi Medical Center (Kusatsu City, Shiga Prefecture) became the first in Japan to introduce a command center, a system for comprehensively collecting and analyzing large amounts of medical data, which has resulted in improved nurse work efficiency and bed occupancy rates. We spoke to Sanae Inami, Director of Nursing, about the background to the introduction of the command center, how electronic medical record data is being used, and the changes in work since its introduction.
I have always felt that we could improve the efficiency of nursing work by making better use of the information in electronic medical records. For example, we used to use a calculator every day to calculate the number of nurses that should be assigned to a ward based on the number of admissions and discharges, but if this could be automated, we would be able to use that time for other tasks, and I had discussed this wish with the hospital's director of business administration.
The head of business administration visited the command center at Johns Hopkins Hospital during a training session in the US for the Japanese subsidiary of a medical device manufacturer, and recommended introducing it to our hospital, saying that it could solve the issues I often talk about.The management team also agreed, and the decision was made to introduce it in 2019.
A command center is a system that integrates information within a hospital, such as electronic medical records, performs comprehensive analysis, and displays necessary information in real time, such as bed occupancy, care, tasks, and staffing.
The Johns Hopkins Hospital command center was a system for regional medical care that primarily visualized ambulance operations and staff deployment. In order to adapt the system for Japanese hospital medical care, we spent six months building an original system while reviewing work processes and gaining the understanding of medical equipment manufacturer personnel who are not medical professionals. When the system first started operating, we had trouble storing and retrieving electronic medical record data, and it took another six months or so to make adjustments.

The command center is located in the conference room where the ward head nurse holds a bed control meeting every morning.
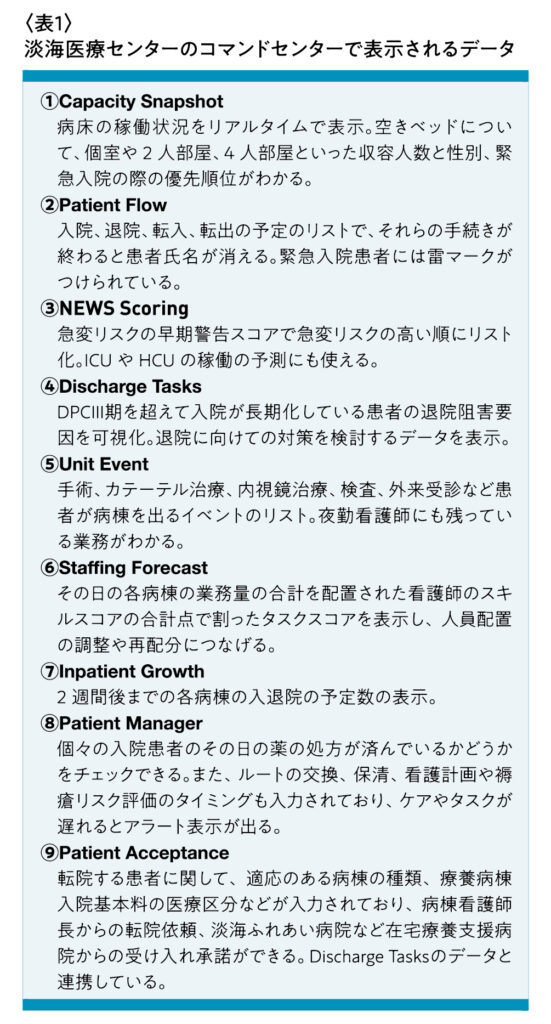
The command center is comprised of a data integration analysis server and multiple applications called tiles. These tiles analyze and visualize the in-hospital data required for bed management and admission/discharge support, and aim to enable medical professionals to provide high-quality, speedy care by capturing ever-changing patient conditions in a timely manner, including care demand predictions, transfers between facilities, care progress, and discharge plans. The number and type of tiles are modular and can be changed according to the size and needs of the facility. Currently, our hospital has 10 monitors installed, displaying items ① to ⑨ in Table 1. Capacity Snapshot ① uses two screens.
The way ward nurses work has changed dramatically as bed occupancy, care and tasks for each patient or the entire ward, and the number and skills of nurses have become visible.
For example, in ⑥Staffing Forecast, you can view data that integrates the tasks and number of nurses assigned to each ward. This screen lists and scores the number of surgeries, catheterization tests, etc., the number of patients with drains or colostomies, the risk of falls, whether or not they have dementia, and the orders for new inpatients. In addition, the task score for each ward is calculated by combining evaluation scores such as the ward nurse's years of experience, position, and ability, and is automatically updated every 15 minutes.
At present, we consider a ward that exceeds a task score of 25 points to be in need of support. As a result, nurses have started to voluntarily go from wards with low task scores to busier wards with high task scores to provide support, which we believe is one of the biggest results of introducing the command center. Also, by visiting wards outside their responsibility, nurses have been able to incorporate new and improved methods they learn in their own wards and have started to share storage areas for items.
By visualizing work and changing working styles in this way, total overtime hours per month in general acute care wards were reduced by 44% (approximately 1,035 hours per month) in 2021 compared to 2020, before the command center went live, even amid the COVID-19 pandemic. The disparity in overtime hours between wards has also improved. Looking at the standard deviation, the variation, which was previously 240 hours, has now shrunk to 78 hours. In particular, the ward with the highest overtime hours saw a significant reduction, from 764 hours to 331 hours, demonstrating progress in adjusting the workload between wards.
③NEWS Scoring evaluates each patient with an early warning score and lists them in order of the risk of sudden deterioration. This is constantly posted in each ward. Blood pressure and other vital signs are measured by holding a nurse's smartphone over a measuring device, and the results are automatically entered into the electronic medical record, which is reflected in the early warning score. Doctors from the ICU and HCU check the same screen and offer advice, and doctors may also keep an eye on and treat patients outside their care. Utilizing this data has dramatically reduced the deterioration of patients' conditions.
The bed occupancy status can be seen in real time, and the care and tasks required for admissions, discharges, transfers, and admissions are listed. As a result, the bed occupancy rate, which was in the low 90s before the system was introduced, is now over 100%.
The introduction of the command center has brought about various benefits, including improved hospital management and medical safety, reduced overtime for nurses, and smoother admissions, discharges, transfers, and transfers.
Another outcome was that the nurses felt that management now understood how busy they were, and they began to think about how to ensure appropriate working conditions in their own ward and other wards.
In the future, we plan to consider introducing a system that will make it easier for nurses to collect information while making use of the data collected at the command center.