Release date: 2025.07.02
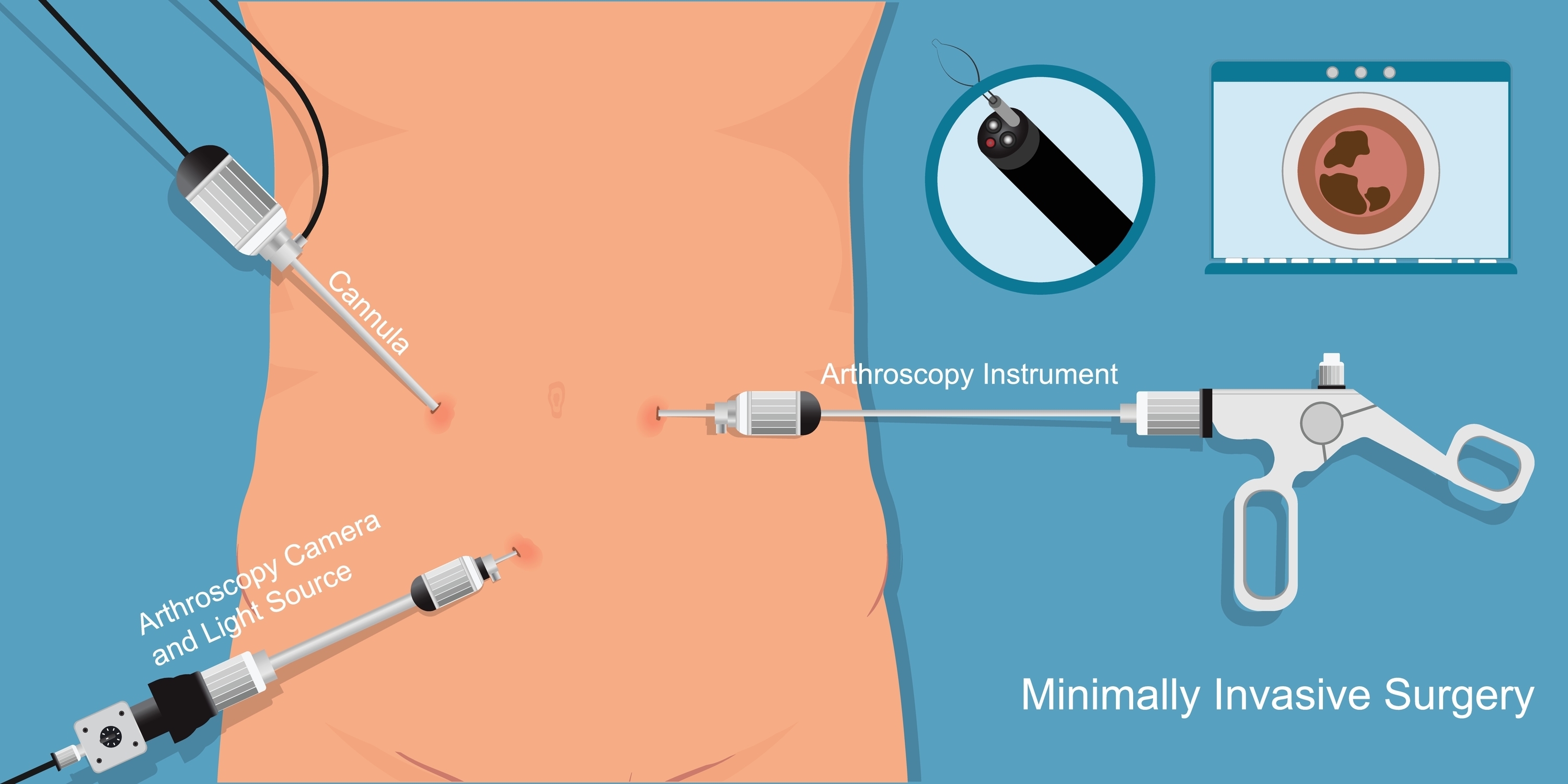
Recently, minimally invasive treatments that reduce the burden on patients have been attracting attention. Compared to traditional open surgery, these treatments are characterized by smaller scars and faster recovery, but there are also issues with their scope of application and cost. In this second installment, we will explain the advantages and limitations of minimally invasive treatments, compare the treatment time and cost with open surgery, and discuss the current state of insurance coverage and future prospects.
The greatest feature of minimally invasive treatments is the reduced burden on patients compared to traditional open or thoracotomy. The most notable advantage of minimally invasive treatments is the shortened recovery period. Because incisions are small and tissue damage is limited, postoperative recovery is faster than with traditional surgery. For example, in the case of cholecystectomy, traditional open surgery requires a hospital stay of approximately one to two weeks, whereas laparoscopic surgery shortens this to approximately two to five days. This allows patients to return to society and daily activities more quickly. Another important benefit is the significant reduction in postoperative pain due to the small incisions and minimal tissue damage. This not only directly improves patients' quality of life (QOL), but also reduces the need for painkillers and the risk of side effects. Studies comparing laparoscopic cholecystectomy with open cholecystectomy have reported lower postoperative pain scores.
Furthermore, minimally invasive treatments are superior from a cosmetic standpoint. While traditional open surgery typically requires an incision of 10 cm or more, laparoscopic surgery allows for surgery with just a few small incisions of about 5–12 mm. Robot-assisted surgery and surgery performed using only a single small port (single-port surgery) further reduce the visibility of scars and the psychological burden on patients. Additionally, minimally invasive treatments reduce the risk of postoperative complications such as wound infection and intestinal obstruction. This benefit is particularly pronounced in elderly patients and those with underlying medical conditions. Data also suggests that laparoscopic surgery reduces wound infections in colorectal cancer surgery compared to open surgery. Furthermore, shorter hospital stays reduce the risk of hospital-acquired infections, thereby improving overall safety.
Minimally invasive treatments also present some challenges and limitations.
First, minimally invasive treatments are not applicable to all cases. For example, traditional open surgery may be chosen in cases where there are severe adhesions, when extensive resection is required for advanced cancer, or when surgery is performed on an anatomically complex area. Furthermore, depending on the patient's overall condition, minimally invasive treatments may not be suitable due to considerations such as pneumoperitoneum (inflating the abdominal cavity with carbon dioxide) and the physiological burden caused by positioning. These limitations on application are important factors in determining the treatment method.
Another challenge is the need for specialized equipment and advanced technology. For example, introducing a robotic surgery system can cost hundreds of millions of yen, and maintenance costs are also high. It also takes time for doctors to become proficient in using it. Without adequate training, the risk of complications can increase. It is said that laparoscopic surgery requires experience with approximately 50 cases to become proficient, but some procedures require even more experience. As a result, the number of facilities and doctors capable of performing advanced minimally invasive treatments is limited. Regional disparities, particularly in rural areas, pose a particular challenge, as there is a shortage of specialists and equipment. This disparity in access to medical care can also affect the quality of care patients receive.
There is a big difference in treatment time and cost between minimally invasive treatment and traditional open surgery.
The length of hospital stay varies depending on the disease, but minimally invasive treatments can often be shorter than traditional open surgery. To give a specific example, colon cancer surgery can be shortened to 7-10 days with laparoscopic surgery, compared to 10-14 days with open surgery. In radical prostatectomy, compared to approximately two weeks with open surgery, there are an increasing number of cases where patients can be discharged in around 7-10 days with robotic-assisted surgery. This shortened hospital stay not only allows patients to return to society sooner, but also contributes to improving hospital bed turnover.
Regarding treatment costs, surgical costs vary depending on the procedure. For example, according to the revision of medical fees for fiscal year 2024, a cholecystectomy costs approximately 277,000 yen for open surgery (approximately 83,000 yen with a 30% co-payment if covered by insurance) compared with approximately 215,000 yen for laparoscopic surgery (approximately 65,000 yen for laparoscopic surgery), making it less expensive. On the other hand, a radical prostatectomy costs approximately 411,000 yen for open surgery (approximately 123,000 yen for laparoscopic surgery) compared with approximately 598,000 yen for robotic-assisted surgery (approximately 179,000 yen for laparoscopic surgery). However, shortening hospital stays reduces overall treatment costs, leading to reduced social security costs, and individual patients can expect economic benefits from earlier return to society.
Under Japan's health insurance system, most minimally invasive treatments are covered by insurance, with patients only paying 30% of the cost (10% or 20% for the elderly). Many laparoscopic surgery procedures are covered by insurance, and robotic-assisted surgery is also used for prostate cancer, kidney cancer, stomach cancer, colon cancer, gynecological cancer, and other cancers. Catheter therapy is also covered by insurance for many cardiac and vascular treatments. However, some advanced minimally invasive treatments may not be covered by insurance, in which case the patient's burden may be greater.
In recent years, the scope of insurance coverage has been expanding, and several new robotic-assisted surgeries have been included in the medical fee revision. This trend is expected to continue, and it is expected that more patients will be able to enjoy the benefits of minimally invasive treatment.
Current challenges in minimally invasive treatment include eliminating regional disparities, establishing education and training systems, and efficiently managing expensive medical equipment. To address these challenges, efforts are being made to promote telemedicine and strengthen cooperation between medical institutions.
Future prospects include the development of navigation systems that utilize AI (artificial intelligence) and VR (virtual reality), further miniaturization and sophistication of equipment, and the practical application of remote surgery. In particular, the widespread use of 5G communications may improve access to advanced medical care in remote islands and rural areas. Furthermore, the development of new minimally invasive treatment technologies is expected to expand the scope of application to diseases and cases that are currently not suitable for use.
MEDIUS Group is developing a business centered on the sale of medical equipment. We (Medical + us) involved in medical care also want to play the role of an information source (Media) that delivers useful information for the medical field and people's healthy tomorrow.