NIH/NCI (National Institutes of Health/National Cancer Institute)
Molecular Imaging Division (Branch) Chief, Molecular Serranostics Laboratory
Director, Institute of Photoimmunology, Kansai Medical University
Hisataka Kobayashi
Graduated from Kyoto University School of Medicine in 1987. After working as a resident in the Department of Radiology, he entered the Department of Internal Medicine Nuclear Medicine at the same graduate school in 1991. Completed the same in 1995 and obtained a doctorate in medicine. In the same year, he moved to the United States and became a visiting researcher in the nuclear medicine department of the NIH Clinical Center. After returning to Japan in 1998, after working as an assistant in the Department of Visual Medicine, Faculty of Medicine, Kyoto University, he returned to the United States in 2001 and worked as a senior fellow at the NIH / NCI Metabolism Laboratory. Since 2004, he has been a Principal Researcher at the NIH / NCI Molecular Imaging Branch.
Cancer photoimmunotherapy developed by Japanese Dr. Hisataka Kobayashi at the National Institutes of Health (NIH). In April 2022, a research center for treatments that are attracting worldwide attention was established in Japan, aiming to cure cancer by irradiating near-infrared rays that attack cancer cells and the power of immunity. We asked Dr. Kobayashi directly about what photoimmunotherapy is, why the research base was set up in Japan, and what kind of research will be carried out there.
In April 2022, the first "Photoimmunotherapy Research Institute" in Japan was established at Kansai Medical University in Hirakata City, Osaka Prefecture. Speaking of cancer treatment, surgery, drug therapy, radiation therapy, and immunotherapy are the four main pillars, but the "photoimmunotherapy" that this photoimmunotherapy research institute intensively studies is the fifth cancer treatment. It has been.
In April 2021, Kansai Medical University opened the "Photoimmunotherapy Center" in the attached hospital prior to the research institute, and is providing treatment for head and neck cancer approved by the Minister of Health, Labor and Welfare. The university has stated that "with the opening of the first research institute in Japan, the two wheels of clinical and research will be aligned, and further improvement of the therapeutic effect and expansion of indications will be promoted."
Cancer photoimmunotherapy was developed at NIH in 2011. The paper was published in the medical journal Nature Medicine in 2011, and was featured in the State of the Union speech (policy speech) by President Obama (then) the following year.
I am still conducting research as a principal investigator of NIH, but this time, I will change the treatment of cancer by the reason for establishing a research base in Japan and how photoimmunotherapy itself will develop in the future. I will explain whether it is. Before that, let's take a look at the principle and current status of cancer photoimmunotherapy.
The principle of cancer photoimmunotherapy itself is very simple.
First, we create an "antibody dye complex" by binding a drug that reacts to light to an antibody that reacts to the antigen exposed on the surface of cancer cells. This is given to cancer patients by intravenous drip, and the drug reaches the cancer cells one day later. Therefore, the principle is that when the tumor site is irradiated with laser light, only the cancer cells to which the antibody dye complex is bound rupture and die.
Many drugs have already been developed and used in actual treatment for antibody therapy targeting cancer cell antigens, but they can also damage normal cells that have the same antigen as the target antigen.
However, in photoimmunotherapy, the amount of drug is small, so the antibody dye complex does not bind to normal cells very much, and "laser light is applied to activate the light-responsive substance attached to the cancer cells." Because it has the advantage of being able to select the location to irradiate with light, it minimizes damage to normal cells and achieves extremely high specificity for cancer.
Moreover, the surrounding immune cells recognize and activate the cancer antigens that have flowed out from the cancer cells destroyed by the antibody dye complex and the laser light attack, thereby inducing the immune cells that attack the cancer cells. .. In other words, after the direct "primary attack" by the antibody complex and laser light, the "secondary attack" that activates the patient's own cancer immunity and attacks the cancer is prepared. (figure)
This first attack eliminates 80% to 90% of cancer cells, but the power of immunity is essential to completely cure the cancer. The surrounding immune cells (T cells) recognize the cancer-specific antigen released from the destroyed cancer cells and attack the surviving cancer cells. The greatest merit of photoimmunotherapy is that it has fewer side effects than conventional treatments, and because it can strongly mobilize the patient's own immune cells in this way, it suppresses the recurrence of cancer and metastasizes. It also has the potential to attack cancer cells that have developed. In the near future, we believe that more than 80% of solid cancers will be indicated for photoimmunotherapy.
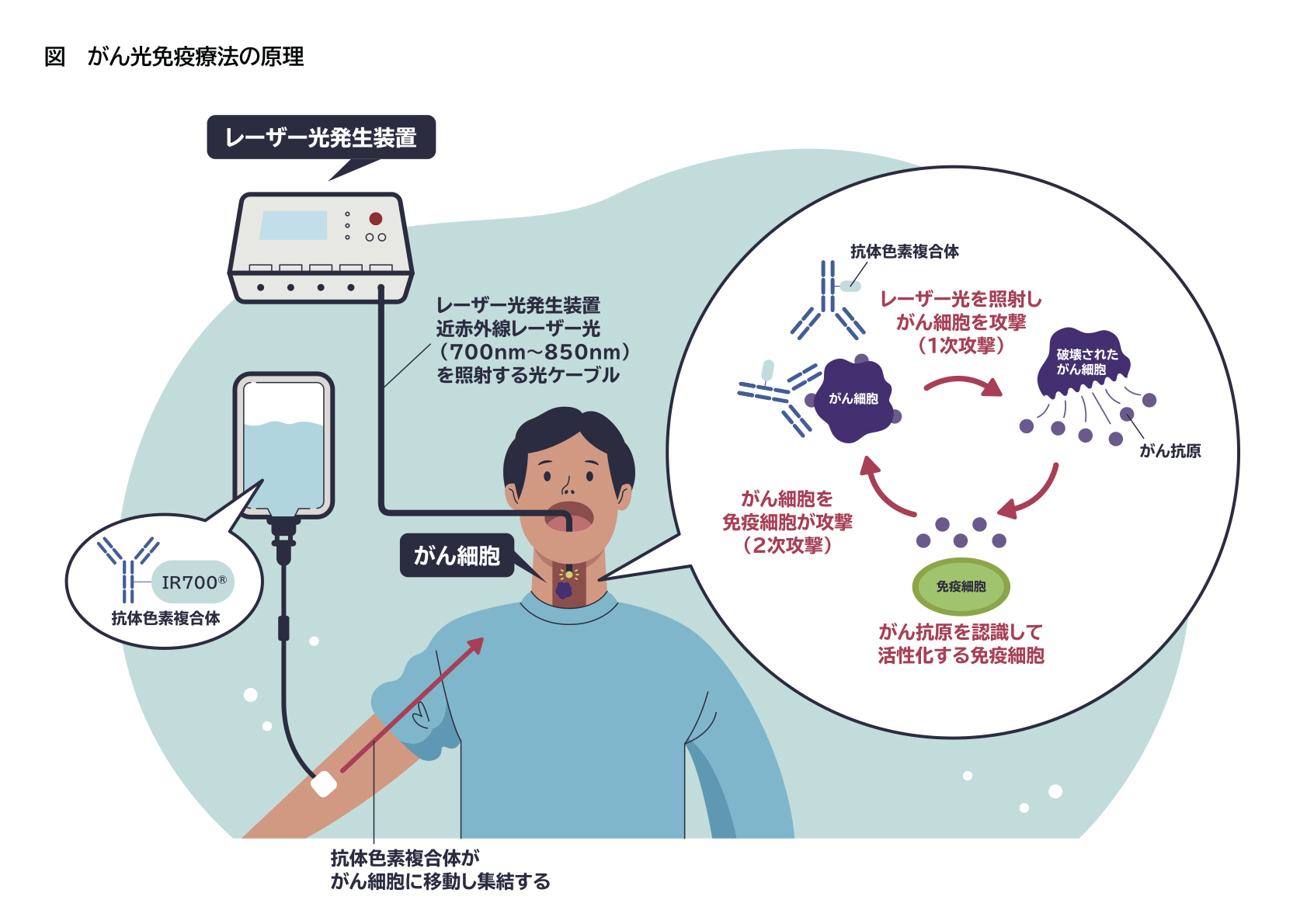
In the "primary attack", the cancer antigen is targeted and the cancer cells are selectively attacked by the antibody dye conjugate and laser light irradiation. The cancer antigen released from the destroyed cancer cells activates the surrounding immune cells and wipes out the slightly surviving cancer cells to establish a "secondary attack".
Clinical development of photoimmunotherapy is progressing by Rakuten Medical Co., Ltd., and in September 2020, both the cancer topical drug "Acalux ® Intravenous Infusion 250 mg" and the medical device laser device "BioBlade ® Laser System" (photo) will be manufactured. After obtaining marketing approval, in November of the same year, it was covered by insurance for "unresectable locally advanced or locally recurrent head and neck cancer", and treatment in Japan began. This was the first practical application in the world.
In fact, one of the reasons for establishing a research base in Japan is that the actual clinical practice was started in Japan for the first time in the world. The data available in clinical practice far surpasses that obtained from clinical studies and clinical trials conducted under many constraints. Since it is a new treatment method, if we can collect realistic data from actual clinical practice, we can reduce it to improvement of treatment. Although it is subject to priority review in the United States, it has not been approved, and it can be said that Japan has overtaken the United States.
Also, as mentioned earlier, Kansai Medical University has already set up a photoimmunotherapy center in 2021. Professor Dai Iwai of the Department of Otorhinolaryngology and Head and Neck Surgery of the University Hospital has been appointed as the director of the center, and we are collecting cases of head and neck cancer. With this, we can expect the "two wheels of clinical and research" that Kansai Medical University calls.
In order to make effective use of the information obtained from actual clinical practice, the Photoimmunotherapy Research Institute has established the "Basic Development Department", "Immune Department", and "Tumor Pathology Department". The plan is to collect immune information and pathological specimens obtained from blood, etc., compare them before and after treatment, and use them to improve treatment policies and techniques later.
 (Photo) BioBlade® Laser System
(Photo) BioBlade® Laser System
In order for future photoimmunotherapy to evolve into a treatment with a higher cure rate for more cancers, research from two aspects is necessary. One is the enhancement of immunity, and the other is the improvement of medical equipment that accurately irradiates the deeper part of the body with laser light.
In order to enhance immunity, it is necessary to make T cells, which are the bearers of the immune system, work efficiently, so the key is to use it in combination with a substance (T cell growth factor) that proliferates and prolongs T cells such as interleukin 15. I'm holding it.
On the other hand, there are immune checkpoint molecules that suppress excessive immune responses and regulatory T cells (Tregs) that suppress the action of T cells in the body. In other words, it is necessary to increase the number of effective T cells and eliminate those that suppress the action of T cells. For the former, it is necessary to use T cell growth factor in combination with photoimmunotherapy, and for the latter, it is necessary to consider the introduction of drugs that inhibit immune checkpoint molecules and new antibody dye complexes targeting Treg. there is.
Improving medical equipment is also important. Lasers used in photoimmunotherapy do not need high power lasers, low power diode lasers are sufficient. Therefore, "how to shine light" is more important than "intensity of light source".
In the future, in order to target cancers that occur inside the body such as pancreatic cancer and bile duct cancer, advances in technology for accurately installing a light source near cancer cells in the body and lasers for cancer cells The optical fiber itself that irradiates the cancer must be improved. I think that it is necessary to prepare optical fibers with various irradiation ranges according to the patient's situation, and the catheter used for insertion also needs the idea of personalized medicine.
Fortunately, there are many top runners in medical equipment and materials in Japan, so we are working with various domestic companies that have top runners to improve laser irradiation technology.
In April 2022, Rakuten Medical announced that "the number of facilities that can provide photoimmunotherapy to the head and neck (head and neck aluminox treatment) has expanded to 62 facilities in 32 prefectures." Following the training program sponsored by the company, the number of doctors who meet the doctor requirements for this treatment has increased to 165.
It is a treatment method that is only allowed by doctors who have limited facilities and special knowledge, but I think that it will be possible to treat it at clinics and dentists in the city in the future. Since the equipment that irradiates the laser beam is already small and portable, it can be used by clinics and dentists if the adaptation to the first healthy patient can be expanded. In some cases, oral cancer is treated by dentists, and we would like to continue improving photoimmunotherapy so that it can be used not only by doctors but also by dental teachers.